For the past 6 months I have been interning at a treatment center for substance abuse. Our center offers outpatient and intensive outpatient (day treatment several days a week) primarily to people who have been court-mandated to seek treatment. There are several reasons someone might seek treatment: to restore their full driving privileges, to regain custody of their children, to avoid a prison sentence because of a DUI or drug possession conviction, or because they have been offered mental health support in lieu of punitive action. We also have self-referred clients who simply realized that their previous attempted solutions have all failed and they need some support to stop using.
Over the course of my internship I have gained an incredible respect for both clients and the healers and helpers who do this work. I have also learned a great deal about substance use, substance use disorder, abstinence, recovery, and evidence-based treatments. I would like to share with you some common myths about substance use (disorder) that have been busted during my time doing this work.
1. “There’s no hope for them.”
There are at least a dozen evidence-based treatments for Substance Use Disorder (SUD), including medication-assisted therapy, cognitive behavioral therapy, motivational enhancement therapy, brief strategic therapy, multi-dimensional family therapy, contingency management, and 12-step facilitation. There is always hope and there are resources to help you in supporting a loved one through treatment.
2. “They have to want to change.” Or “They have to hit rock bottom before they’ll stop using.”
Actually, mandated treatment works (I’ve seen it!) and people with an addiction are likely to enter treatment because they have a concerned significant other, more than because they’ve hit “rock bottom”; “family influence is the most commonly cited reason for treatment entry among help-seeking substance user” (Foote & Rosenbaum, 2009). An approach called Community Reinforcement and Family Training (CRAFT) has been proven effective. Research on CRAFT shows that about 70% of families who receive CRAFT are able to get their loved ones into treatment within a year. You can help your loved one better themselves. If you or someone you love could benefit from support, you can call the SAMHS National Hotline 1-800-662-HELP (4357).

3. “Once an addict, always an addict.”
This misconception is potentially very harmful to people in recovery and it doesn’t capture the whole picture. The medical model of looking at addiction tells us that SUD is a disease and it is one that has no conventional cure. Once someone experiences chemical dependence, the chronic nature of the disease means that their brain and body will need continued care to prevent relapse. But, let’s consider other diseases and ask ourselves, “Why is addiction is one of few diseases that people get blamed for having?” The shame and judgment surrounding addiction only exacerbates barriers to seeking treatment. Compassion and empathy go a long way in restoring someone’s self-esteem and empowerment.
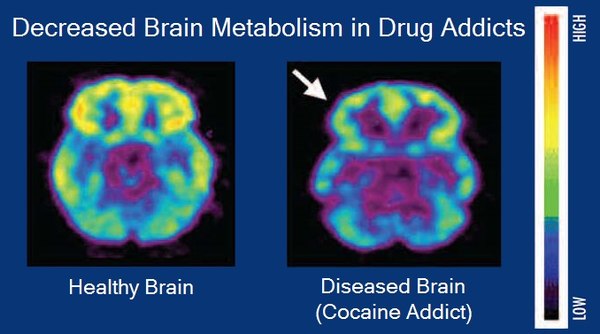
4. “You can just choose not to use.” Or “Why don’t you just quit?” The collusion of our biochemistry and neurobiology is easily manipulated by addictive substances, and for some people (for any number of reasons) at some point, the disease will begin making the decisions. Once a substance begins to penetrate the barrier between the bloodstream dedicated to the brain and the bloodstream of the rest of the body, the mind’s ability to understand rewards, risks, and decision-making is compromised. The brain is unable to provide the kind of weighing of consequences that is necessary to choose not to use the substance again. What’s tragic is that stress—a compelling reason someone might turn to substances—makes this blood-brain barrier more permeable so the drugs can have a more intense effect depending upon the context in which they are used. The idea of choice to quit using a substance is a misunderstanding from the moral model of addiction, which modern medicine abandoned over 90 years ago; it’s time the rest of society gave it up too.
5. “People who turn to alcohol or drugs to cope are just weak.” Well, given what we know about how drugs hijack our neurobiology and how stress can make the whole matter worse, the question we should really be asking is, “Why don’t more people use drugs to cope?” In the 1970s, a researcher by the name of Bruce Alexander conducted experiments on rats to learn more about addictive behaviors. The rats were given two sources of water: plain water and water with morphine The rats chose the laced bottles consistently—some to the point of overdosing, affirming the habitual nature of the substance use. But then Alexander considered the context. Humans are complex, social creatures and are rarely using substances in isolation. So he created a rat park, a shared community of rats living together where they could socialize, play, and procreate. The results were astonishing: the rats rarely drank from the laced bottles once they were moved to rat park and those that did only imbibed episodically, without overdosing. Alexander’s experiment complicated our understanding of even the disease model of addiction and gave rise to the idea that the opposite of addiction is quality connection. People don’t turn to drugs or alcohol because they are weak; they use because they are in unbearable physical, emotional, or spiritual pain.
Enduring life’s challenges is a universal aspect of the human experience. In the field of helping and healing, we use person-centered care to ensure that no client is left feeling judged, shamed, or misunderstood. Several resources were shared in this blog and there are countless more. Remember, there is hope for you or your loved one. You don’t have to endure addiction alone.